Chronic Kidney Disease: Understanding the Silent Epidemic
Table of Contents
Introduction
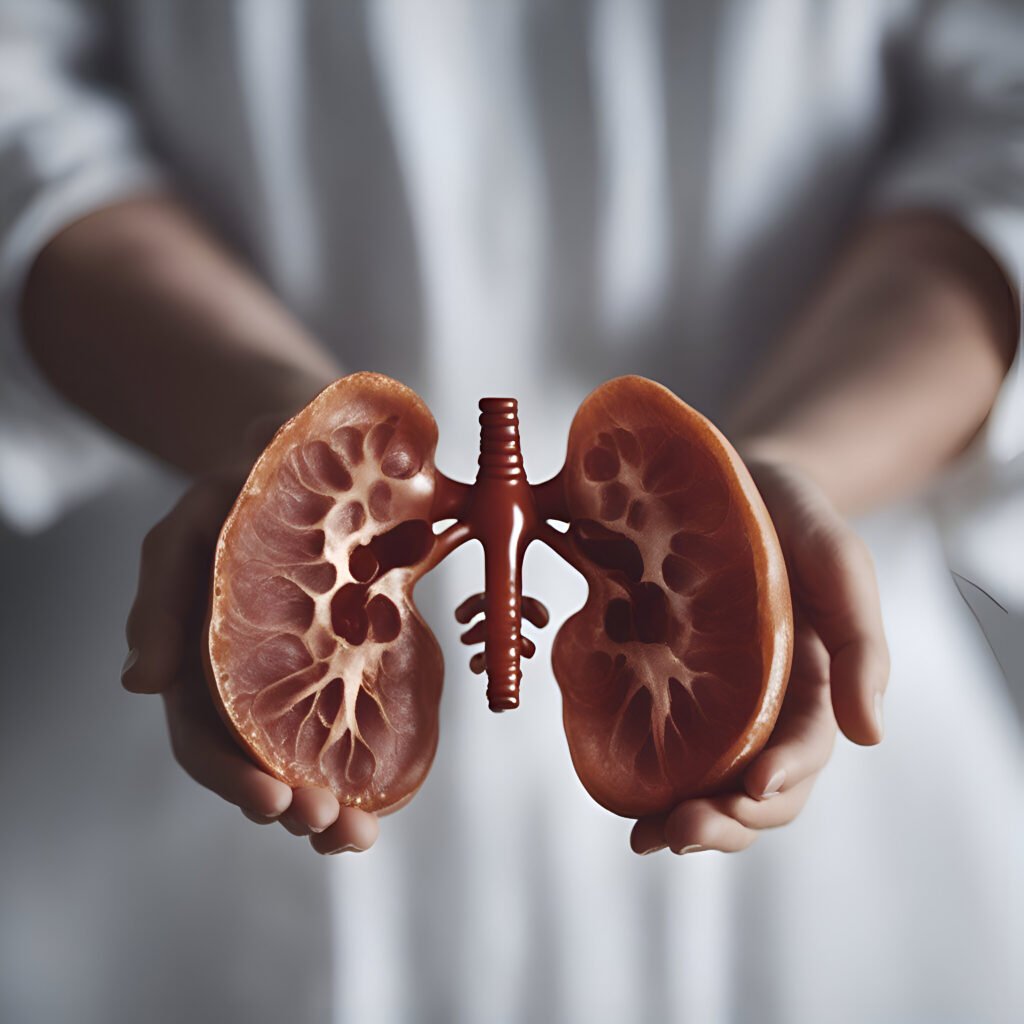
Chronic Kidney Disease (CKD) is a pervasive and increasingly prevalent health issue that has garnered global attention due to its substantial impact on individuals and healthcare systems worldwide. Characterized by the gradual and irreversible deterioration of kidney function over time, CKD poses a significant burden on affected individuals, their families, and society as a whole. Despite its profound implications for health and well-being, CKD often remains underdiagnosed and undertreated, particularly in its early stages when symptoms may be subtle or absent.
This comprehensive guide aims to provide a thorough examination of CKD, encompassing its definition, various forms, historical context, prevalence and demographic patterns, symptomatic manifestations, available treatment options, preventative strategies, and concluding insights. By shedding light on the complexities of CKD, we hope to raise awareness about this silent yet impactful condition and emphasize the importance of early detection, proactive management, and public health interventions in mitigating its effects.
Concept of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a progressive and irreversible condition characterized by the gradual loss of kidney function over time. The kidneys play a crucial role in filtering waste products and excess fluids from the blood, regulating blood pressure, and maintaining electrolyte balance in the body. In CKD, the kidneys become damaged and are unable to perform these functions effectively, leading to a buildup of waste products and fluids in the body.
CKD is typically classified into five stages based on the estimated glomerular filtration rate (eGFR), which measures how well the kidneys are filtering waste from the blood. Stage 1 CKD is the mildest stage, with a slightly reduced eGFR, while stage 5 CKD, also known as end-stage renal disease (ESRD), is the most severe, with a significantly reduced eGFR requiring kidney replacement therapy such as dialysis or transplantation.
CKD can be caused by a variety of factors, including diabetes, hypertension, glomerulonephritis, and polycystic kidney disease. Each of these conditions can damage the kidneys and lead to CKD if not properly managed. CKD is a progressive condition, meaning that it tends to worsen over time if left untreated. However, early detection and treatment can help slow the progression of the disease and reduce the risk of complications.
It is important to note that CKD is often asymptomatic in its early stages, making it challenging to diagnose. As the disease progresses, symptoms such as fatigue, swelling in the legs, foamy urine, and changes in urination patterns may occur. Regular screening tests, including blood and urine tests, are essential for detecting CKD early and initiating appropriate treatment.
Overall, CKD is a complex and multifaceted condition that requires comprehensive management to preserve kidney function and improve quality of life. By understanding the concept of CKD and its underlying causes, healthcare providers can work towards early detection, timely intervention, and optimal management of this chronic condition.
Variations of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a progressive and irreversible condition characterized by the gradual loss of kidney function over time. The kidneys play a crucial role in filtering waste products and excess fluids from the blood, regulating blood pressure, and maintaining electrolyte balance in the body. In CKD, the kidneys become damaged and are unable to perform these functions effectively, leading to a buildup of waste products and fluids in the body.
CKD is typically classified into five stages based on the estimated glomerular filtration rate (eGFR), which measures how well the kidneys are filtering waste from the blood. Stage 1 CKD is the mildest stage, with a slightly reduced eGFR, while stage 5 CKD, also known as end-stage renal disease (ESRD), is the most severe, with a significantly reduced eGFR requiring kidney replacement therapy such as dialysis or transplantation.
CKD can be caused by a variety of factors, including diabetes, hypertension, glomerulonephritis, and polycystic kidney disease. Each of these conditions can damage the kidneys and lead to CKD if not properly managed. CKD is a progressive condition, meaning that it tends to worsen over time if left untreated. However, early detection and treatment can help slow the progression of the disease and reduce the risk of complications.
It is important to note that CKD is often asymptomatic in its early stages, making it challenging to diagnose. As the disease progresses, symptoms such as fatigue, swelling in the legs, foamy urine, and changes in urination patterns may occur. Regular screening tests, including blood and urine tests, are essential for detecting CKD early and initiating appropriate treatment.
Overall, CKD is a complex and multifaceted condition that requires comprehensive management to preserve kidney function and improve quality of life. By understanding the concept of CKD and its underlying causes, healthcare providers can work towards early detection, timely intervention, and optimal management of this chronic condition.
Historical Context
The understanding and management of Chronic Kidney Disease (CKD) have evolved significantly over the centuries, reflecting advancements in medical knowledge and technology. Here is a brief overview of the historical context of CKD:
- Ancient Times: The concept of kidney disease dates back to ancient civilizations such as Egypt, Greece, and India. Ancient texts describe symptoms resembling kidney disease and suggest treatments such as herbal remedies and dietary modifications.
- Middle Ages: During the Middle Ages, kidney disease was often associated with urinary symptoms and was sometimes attributed to supernatural causes. Treatment methods included bloodletting and herbal concoctions.
- 18th and 19th Centuries: The understanding of kidney disease began to advance during the 18th and 19th centuries, with physicians such as Richard Bright making significant contributions to the field. Bright’s disease, a term used to describe kidney disease, was named after him.
- 20th Century: The 20th century saw major advancements in the diagnosis and treatment of kidney disease. The development of techniques such as kidney biopsy and the introduction of hemodialysis and kidney transplantation revolutionized the management of CKD.
- Modern Era: In recent decades, there has been a greater focus on early detection and prevention of CKD. Guidelines and screening programs aim to identify individuals at risk and intervene early to slow the progression of the disease.
- Research and Innovation: Ongoing research continues to improve our understanding of the pathophysiology of CKD and develop new treatment modalities. Genetic studies, biomarker research, and advances in imaging technology are shaping the future of CKD management.
- Global Impact: CKD is now recognized as a global health issue, with the World Health Organization (WHO) highlighting the need for strategies to address the growing burden of kidney disease worldwide.
Overall, the historical context of CKD reflects a journey of discovery and innovation, leading to significant improvements in the diagnosis, treatment, and prevention of this complex condition. Ongoing efforts are needed to further advance our understanding of CKD and improve outcomes for patients affected by this disease.
Incidence and Demographic Data
Chronic Kidney Disease (CKD) is a widespread health issue that affects people of all ages, races, and socioeconomic backgrounds. Understanding the incidence and demographic data of CKD is crucial for developing effective prevention and treatment strategies. Here is a detailed overview of the incidence and demographic patterns of CKD:
- Global Burden: CKD is a global health concern, with an estimated prevalence of around 10% worldwide. The burden of CKD varies by region, with higher rates reported in low- and middle-income countries.
- Age: CKD is more common in older adults, with the prevalence increasing with age. However, CKD can affect individuals of all ages, including children and adolescents.
- Gender: CKD affects both men and women, but some studies suggest that men may have a slightly higher risk of developing CKD compared to women. The reasons for this gender difference are not fully understood and may vary depending on the underlying causes of CKD.
- Race and Ethnicity: Certain racial and ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher prevalence of CKD compared to other groups. This disparity is thought to be due to a combination of genetic, socioeconomic, and environmental factors.
- Socioeconomic Status: Socioeconomic status is a significant determinant of CKD risk, with individuals from lower socioeconomic backgrounds being more likely to develop CKD. Factors such as limited access to healthcare, unhealthy lifestyle habits, and exposure to environmental toxins contribute to this disparity.
- Comorbidities: CKD often coexists with other chronic conditions, such as diabetes, hypertension, and cardiovascular disease. These comorbidities can increase the risk of CKD and worsen its outcomes.
- Global Trends: The global prevalence of CKD is expected to rise in the coming years due to aging populations, increasing rates of diabetes and hypertension, and changes in lifestyle factors such as diet and physical activity.
Understanding the incidence and demographic data of CKD is essential for developing targeted interventions and policies to reduce the burden of this disease. By addressing risk factors and promoting kidney health, we can work towards preventing CKD and improving outcomes for those affected by this condition.
Symptoms of Chronic Kidney Disease (CKD)
Symptoms of Chronic Kidney Disease (CKD) can vary depending on the stage of the disease and the underlying causes. In the early stages, CKD may be asymptomatic, meaning that individuals may not experience any symptoms. However, as the disease progresses, the following symptoms may develop:
- Fatigue: Persistent fatigue and weakness are common symptoms of CKD, often due to anemia (a decrease in red blood cells) and the buildup of waste products in the body.
- Swelling: Swelling, also known as edema, may occur in the legs, ankles, feet, face, or hands due to fluid retention caused by the kidneys’ inability to filter fluids properly.
- Changes in Urination: Individuals with CKD may experience changes in their urination patterns, such as increased or decreased frequency, foamy or bubbly urine, or difficulty urinating.
- Blood in Urine: Hematuria, or blood in the urine, can occur in CKD due to damage to the kidneys’ filtering units (glomeruli).
- High Blood Pressure: CKD can lead to hypertension (high blood pressure), which can further damage the kidneys and increase the risk of cardiovascular disease.
- Loss of Appetite: Individuals with CKD may experience a loss of appetite, nausea, or vomiting, which can contribute to weight loss and malnutrition.
- Itching: Pruritus, or itching, is a common symptom of CKD, believed to be related to the buildup of toxins in the blood.
- Muscle Cramps: Muscle cramps, particularly in the legs, can occur in individuals with CKD, often due to electrolyte imbalances.
- Difficulty Concentrating: CKD can affect cognitive function, leading to difficulty concentrating, memory problems, and overall mental sluggishness.
- Sleep Problems: Individuals with CKD may experience sleep disturbances, such as insomnia or restless legs syndrome, which can further contribute to fatigue and daytime drowsiness.
It is important to note that symptoms of CKD can be nonspecific and may overlap with other conditions. Therefore, if you experience any of these symptoms, it is essential to consult with a healthcare professional for a proper evaluation and diagnosis. Early detection and management of CKD can help slow the progression of the disease and improve outcomes.
Treatment of Chronic Kidney Disease (CKD)
Treatment of Chronic Kidney Disease (CKD) aims to slow the progression of the disease, manage symptoms, and prevent complications. The treatment approach may vary depending on the stage of CKD and the underlying causes. Here are some key aspects of CKD treatment:
- Blood Pressure Control: Managing high blood pressure is crucial in slowing the progression of CKD. This may involve lifestyle changes (such as diet and exercise) and medications (such as ACE inhibitors or ARBs) to lower blood pressure.
- Blood Sugar Control: For individuals with diabetes, controlling blood sugar levels is essential in managing CKD. This may involve medications, insulin therapy, and lifestyle modifications.
- Protein Restriction: Limiting protein intake can help reduce the workload on the kidneys and slow the progression of CKD. A dietitian can provide guidance on the appropriate amount of protein for individuals with CKD.
- Fluid Management: Individuals with CKD may need to restrict their fluid intake to avoid fluid buildup in the body. This is especially important for those with advanced CKD or on dialysis.
- Electrolyte Balance: CKD can lead to imbalances in electrolytes such as potassium, phosphorus, and calcium. Monitoring and managing these electrolyte levels are crucial in CKD treatment.
- Medication Management: Depending on the stage of CKD and the underlying causes, medications may be prescribed to manage symptoms, control blood pressure, and treat complications such as anemia and bone disease.
- Dialysis: In advanced stages of CKD (usually stage 5), when the kidneys are no longer able to function effectively, dialysis may be necessary. Dialysis involves using a machine to filter waste products and excess fluids from the blood.
- Kidney Transplantation: For some individuals with advanced CKD, kidney transplantation may be an option. A donated kidney can replace the function of the failed kidneys, offering a more permanent solution compared to dialysis.
- Lifestyle Modifications: Quitting smoking, maintaining a healthy weight, exercising regularly, and eating a balanced diet are essential in managing CKD and reducing the risk of complications.
- Regular Monitoring: Regular monitoring of kidney function, blood pressure, blood sugar levels, and electrolyte levels is crucial in managing CKD and adjusting treatment as needed.
It is important for individuals with CKD to work closely with their healthcare team, which may include a nephrologist, dietitian, and other healthcare professionals, to develop a comprehensive treatment plan tailored to their specific needs and stage of CKD. Early detection, proactive management, and lifestyle modifications can help improve outcomes and quality of life for individuals living with CKD.
Prevention of Chronic Kidney Disease (CKD)
Prevention of Chronic Kidney Disease (CKD) focuses on addressing risk factors and promoting kidney health to reduce the likelihood of developing CKD. Here are some key strategies for preventing CKD:
- Manage Underlying Conditions: Controlling conditions such as diabetes and hypertension can help prevent or delay the onset of CKD. This may involve medication, lifestyle changes, and regular monitoring.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support kidney health. Limiting sodium, sugar, and processed foods can also help prevent CKD.
- Stay Hydrated: Drinking plenty of water helps the kidneys flush out toxins and waste products. However, individuals with CKD or certain kidney conditions may need to limit fluid intake, so it’s essential to consult with a healthcare provider.
- Regular Exercise: Engaging in regular physical activity can help maintain a healthy weight, reduce blood pressure, and improve overall health, which can lower the risk of developing CKD.
- Avoid Smoking: Smoking can damage blood vessels and increase the risk of kidney disease. Quitting smoking can improve overall health and reduce the risk of CKD.
- Limit Alcohol Consumption: Excessive alcohol consumption can contribute to kidney damage. Limiting alcohol intake to moderate levels is advisable for kidney health.
- Manage Medications Carefully: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can harm the kidneys if used excessively. It’s essential to use medications as directed and consult with a healthcare provider before starting any new medications.
- Regular Health Check-ups: Regular health check-ups, including blood pressure, blood sugar, and kidney function tests, can help detect and manage risk factors for CKD early.
- Maintain a Healthy Weight: Obesity is a risk factor for CKD. Maintaining a healthy weight through diet and exercise can help prevent CKD and its complications.
- Awareness and Education: Increasing awareness about CKD risk factors, symptoms, and preventive measures can empower individuals to take proactive steps to protect their kidney health.
By incorporating these preventive measures into daily life, individuals can reduce their risk of developing CKD and promote overall kidney health. Early detection and management of risk factors are key in preventing CKD and its complications.
Conclusion
Chronic Kidney Disease (CKD) is a significant health issue with far-reaching implications for individuals and healthcare systems worldwide. While the prevalence of CKD continues to rise, there is hope in the growing understanding of its risk factors, prevention strategies, and treatment options. This comprehensive guide has explored the complexities of CKD, from its definition and variations to its historical context, incidence, demographic data, symptoms, treatment, and prevention.
It is evident that CKD is a multifaceted condition that requires a multidisciplinary approach to management. Early detection and intervention, along with lifestyle modifications and adherence to treatment plans, can significantly slow the progression of CKD and improve outcomes for those affected. Additionally, efforts to raise awareness, promote kidney health, and reduce modifiable risk factors are essential in the fight against CKD.
It is crucial for individuals to prioritize their kidney health by adopting healthy lifestyle habits, managing underlying conditions, and seeking regular medical check-ups. By taking proactive steps to prevent and manage CKD, individuals can reduce their risk of complications and improve their quality of life.
Lastly, while this guide provides valuable information about CKD, it is important to remember that it is not a substitute for professional medical advice. Individuals with concerns about their kidney health should consult with a healthcare provider for personalized guidance and care. Together, we can work towards a future where CKD is better understood, more effectively managed, and ultimately prevented.
See more in The 10 Most Common Diseases Affecting Humans Worldwide